the oxygenation continuum
The primary goal of airway management is to maintain tissue oxygenation so as to prevent patients from suffering hypoxic injury. While techniques exist which allow airway management without the occurrence of apnoea/airway obstruction, these may not always be successful or clinically appropriate. Additionally, these techniques are usually only implemented when a challenging airway is anticipated, and as such, have limited utility in the management of the unanticipated challenging airway. Thus the risk of an interruption to alveolar oxygen delivery and subsequent hypoxic harm, is inherently involved with the process of airway management in both the elective and emergency situation.
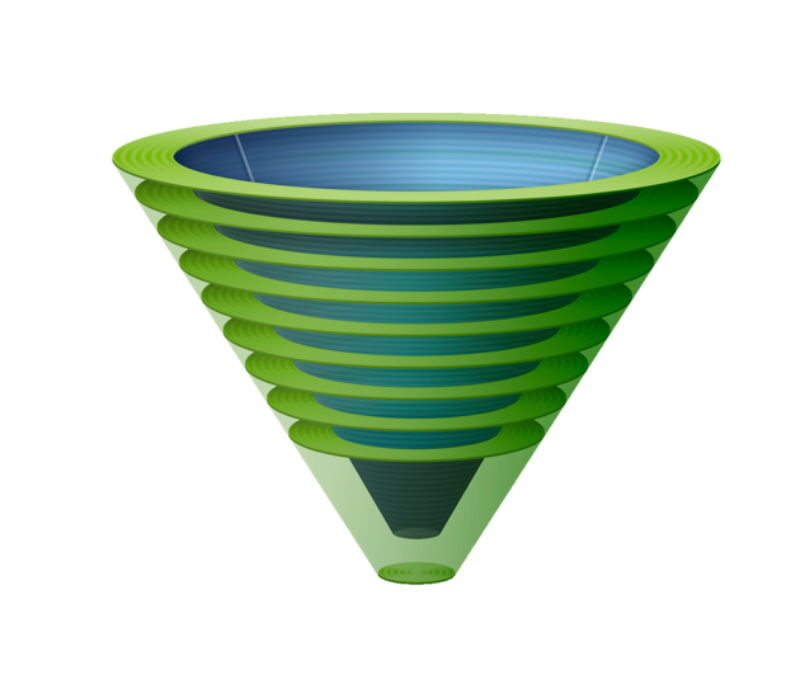
When apnoea/obstruction occurs, oxygen delivery to the alveoli must be restored before critical desaturation occurs in order to avoid the risk of hypoxic injury. Two complementary strategies are available to preserve tissue oxygenation and reduce the risk of patients suffering hypoxic injury:
Establishing alveolar oxygen delivery: is the definitive strategy to preserve tissue oxygenation. A sustained interruption to alveolar oxygen delivery will eventually inevitably lead to decreases in blood oxygen content (“blood oxygenation”) and delivery of oxygen to the tissues (“tissue oxygenation”). Interruptions to tissue oxygenation which are sufficiently prolonged or severe will result in hypoxic injury to the patient. Establishment of alveolar oxygen delivery is represented in the Vortex Approach by entry into the Green Zone.
Extending the safe apnoea time: is a supplementary strategy that can prolong the time until blood and tissue oxygenation decreases in the event that alveolar oxygen delivery by ventilation/insufflation is transiently interrupted (safe apnoea time). If alveolar oxygen delivery is not restored, however, the patient will still eventually falls in blood and tissue oxygenation to dangerous levels. Extending the safe apnoea time merely delays critical desaturation and provides time to implement the definitive strategy that will ultimately prevent/reverse desaturation. It is thus an adjunct, not an alternative, to restoring alveolar oxygen delivery.
“Extending the safe apnoea time merely delays critical desaturation and provides time to implement the definitive airway strategy that will ultimately prevent/reverse desaturation. It is thus an adjunct, not an alternative, to restoring alveolar oxygen delivery.”
Whilst other factors such as gas exchange, haemoglobin concentration and blood flow may also impact tissue oxygenation, these are not influenced by the interventions associated with airway management. Thus it is important to recognise that maintenance of normal oxygen saturations is not synonymous with entry into the Green Zone. Normal oxygen saturations may be maintained within the safe apnoea time despite the absence of ongoing alveolar oxygen delivery. Conversely factors influencing gas exchange or cardiac output may lead to compromise of oxygen saturations despite the presence of alveolar oxygen delivery. Note that the term "alveolar oxygenation" has been avoided due to ambiguity over whether it refers to delivery of fresh oxygen to the alveoli (alveolar oxygen delivery) or maintenance of high alveolar concentrations (which may occur due to effective preoxygenation despite airway obstruction and an interruption to alveolar oxygen delivery).
The concept of the oxygenation continuum provides a visual representation describing the relationship between techniques to establish alveolar oxygen delivery and techniques to prolong the safe apnoea time in minimising the risk of exposing patients to hypoxic injury.
Under routine circumstances the time taken to establish entry into the Green Zone is shorter than the time for critical desaturation, providing a margin of safety for airway management during which the oxygenation continuum is maintained, avoiding exposing the patient to critical hypoxia. The actual time available until critical desaturation occurs if alveolar oxygen delivery is interrupted is only known retrospectively but there are a number of patient factors which might influence it including:
- Body habitus: obesity, pregnancy and other factors which decrease the size of the functional residual capacity may limit the safe apnoea time.
- Increased oxygen consumption: e.g. sepsis, pregnancy, paediatrics may decrease the safe apnoea time
- Impaired gas exchange: respiratory disease may decrease safe apnoea time
- Decreased blood oxygen carrying capacity: anaemia may decrease safe apnoea time
- Decreased cardiac output: may lead to increased oxygen extraction, lower mixed venous oxygen content, increased alveolar oxygen uptake and a lower oxygen content of any shunted blood - all of which will tend to depress the arterial oxygen saturations.
- Techniques to increase the safe apnoea time: preoxygenation, reoxygenation, apnoeic oxygenation, conserving oxygenation
Similarly the time taken to establish alveolar oxygen delivery is unknown prospectively but may be influenced by a number of patient, situational or clinician factors. These are outlined in relation to airway assessment.
If the safe apnoea time is shortened &/or the time to entry into the Green Zone prolonged, the margin of safety is reduced. If this occurs to a sufficient extent the oxygenation continuum may be interrupted, exposing the patient to critical hypoxia.
Minimising the risk of exposing the patient to prolonged hypoxia necessitates maximising the safe apnoea time and minimising the time to enter the Green Zone so as to optimise the margin of safety and decrease the chance of interruption to the oxygenation continuum.
- The Vortex Approach is directed at minimising the time to gain entry into the Green Zone by establishing alveolar oxygen delivery as efficiently as possible.
- Techniques to prolong the safe apnoea time maximise the time to critical desaturation. These techniques are not part of the Vortex Approach but are valuable complementary strategies that should be utilised with it in an integrated fashion. The information outlined below in relation to these techniques is based predominantly on the work or Scott Weingart, Richard Levitan, Anil Patel and Andrew Heard.
“Extending the safe apnoea time thus makes contributions to both technical and human factors considerations that can decrease the risk of patient hypoxia during airway management”
Delaying desaturation by extending the safe apnoea time not only reduces the risk of exposing the patient to hypoxia while airway interventions are performed but also makes an important psychological contribution, decreasing clinician stress and thereby potentially improving both cognitive and motor function during airway management. These improvements act synergistically with the principles of the Vortex Approach to augment the quality of any interventions by improving both decision making and technical skills and thus the likelihood of success at establishing alveolar oxygen delivery by either the upper airway lifelines or CICO Rescue. Extending the safe apnoea time thus makes contributions to both technical and human factors considerations that can decrease the risk of patient hypoxia during airway management.