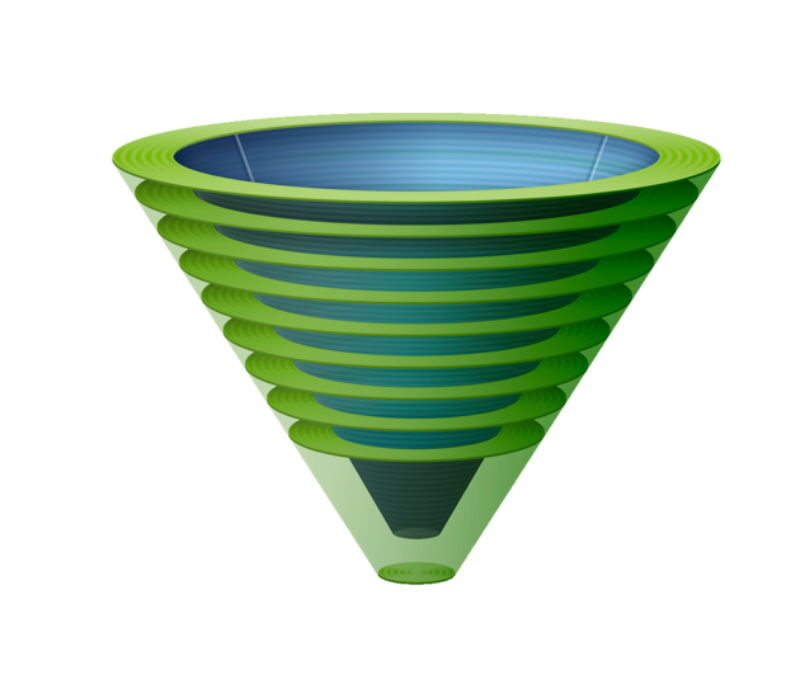
Upper airway lifelines
When successful, the three upper airway lifelines of face mask (FMV), supraglottic airway (SGA) and endotracheal tube (ETT) are equally able to fulfil the goal of alveolar oxygen delivery but differ in their ability to fulfil secondary goals such as airway protection, airway security, and carbon dioxide elimination. Whilst important, these secondary goals become inconsequential if alveolar oxygen delivery cannot be achieved.
In routine circumstances, achieving alveolar oxygen delivery simply involves using a lifeline which has been selected to satisfy both the primary and secondary airway management goals necessitated by the clinical situation. When airway management becomes challenging, however, secondary goals may have to be compromised to ensure alveolar oxygen delivery is achieved.
The Vortex Approach allows clinicians the flexibility to initiate airway management using whichever lifeline is felt to be most appropriate to the clinical situation. If initial attempts to establish alveolar oxygen delivery are challenging, the remaining lifelines can also be implemented in whatever sequence is deemed most appropriate in the clinical circumstances. This flexibility in the sequence in which lifelines are attempted allows the Vortex to be applied to any context in which airway management occurs.
BEST EFFORTS
The term 'best effort' is used by the Vortex Approach to describe the circumstance in which all viable strategies to facilitate success at entering the Green Zone via a given lifeline have been implemented. Up to three attempts (+/- a 'gamechanger' - see below), each incorporating additional optimisations that have not previously been implemented, are permitted to complete a best effort. The specific optimisations employed and the number of attempts that are appropriate to achieve a best effort are context dependent decisions, to be made by the airway operator within the confines of the principles set out by the Vortex Approach.
If following a completed best effort at a particular lifeline, alveolar oxygen delivery has not been achieved, then no further attempts at that lifeline should occur. Efforts should instead focus on establishing alveolar oxygen delivery via an alternate lifeline - or on initiating Neck Rescue if all three lifelines have been unsuccessful.
optimisations
The Vortex model prompts five categories of optimisation that may be applied to improve success entering the Green Zone via any of the lifelines.
These five categories apply equally to each of the three lifelines. The specific interventions within each category are discussed elsewhere in relation to the individual lifelines. Categorising optimisations in this manner allows the entire team to track what interventions have been implemented by the airway operator and to offer suggestions in a structured way.
It is not intended that all the optimisation interventions in a given category are exhaustively implemented for a particular lifeline - this would be both time consuming and inappropriate in most circumstances. Instead the optimisation headings serve to encourage the clinical team to consider all of the options, with the airway operator only implementing those thought to be beneficial in a particular context. This structured approach to considering optimisation strategies maximises the opportunities for achieving timely entry to the Green Zone by ensuring that the process of achieving a best effort is:
Efficient: by minimising both the time and number of attempts to implement all strategies considered to be useful.
Rigorous: by minimising the likelihood that potentially helpful interventions are overlooked
Defined: by outlining a discrete set of optimisations for a given lifeline and thereby providing an endpoint to optimisation. This promotes team recognition that a best effort at a given lifeline has been completed and the need to move on to an alternate technique if alveolar oxygen delivery has not been achieved.
The goal is to maximise opportunities to enter into the Green Zone in the shortest possible time. This makes optimal use of the safe apnoea time and minimises the risk that the patient will be exposed to critical hypoxia.
Note that the optimisation prompts listed on the Vortex tool focus on strategies that can be implemented in real time during management of the challenging airway. As such there are additional optimisations (e.g. shaving a beard) that are not prompted by the tool which can be incorporated prior to initiating airway management. The following "training matrix" gives an overview of the real-time optimisations that can be implemented for each of the upper airway lifelines. It is not intended as an implementation tool for use during an airway crisis. The impact of each of these interventions (& thus the difficulties with establishing an airway with each of the lifelines that provide the indication for their use) are dealt with in more detail below.
Attempts
Except in extraordinary circumstances, where it is considered that a lifeline has a negligible chance of success in a particular clinical situation (particularly if the patient is already severely hypoxic), at least one attempt at each lifeline is usually indicated prior to initiating CICO Rescue. Although desirable, it is not usually possible to implement all optimisations required to maximise success at a given lifeline and achieve a best effort on the first attempt. Additional factors which might improve the chances of entering the Green Zone may only be identified after initial airway manipulations have taken place.
The Vortex model allows up to three attempts to achieve a best effort at each lifeline but emphasises using the minimum number of attempts required. Limiting the number of attempts at each lifeline is important from two perspectives:
Trauma: repeated instrumentation of the airway has the potential to cause trauma which can compromise subsequent success with any of the lifelines and convert what would otherwise have been a "can oxygenate" situation into a "can't oxygenate" situation. Repeated airway instrumentation in desperation is also known to have caused additional trauma resulting in patient morbidity beyond airway compromise.
Time: repeated airway instrumentation also consumes time, delaying implementation of alternate techniques and potentially increasing the duration and severity of hypoxaemia to which the patient may be exposed before entry to the Green Zone is established.
The definition of an attempt varies according to the lifeline being implemented.
For ETT it is defined as the insertion and removal of laryngoscope from the airway.
For SGA it is defined as the insertion and removal of a supraglottic airway from the airway.
For FMV it is defined as the application and removal of a face mask to the patient's face in association with intervening generation of positive pressure with the intent of achieving alveolar ventilation
It is not necessary that all attempts in pursuit of a best effort at one lifeline must be completed before initiating the first attempt at an alternate lifeline. In keeping with normal clinical practice, best efforts at multiple different lifelines may be proceeding in parallel, with sequential attempts alternating between optimising different lifelines. Thus the Vortex implementation tool tracks 'completed best efforts' at each lifeline rather than the sequence of individual attempts required to achieve them.
CLINICAL INTEGRATION
The structured approach to considering optimisation strategies using the five categories of the Vortex for each lifeline can be made even more effective by integrating this approach into the clinical environment. Labelling the emergency airway cart drawers to correspond to the different zones of the Vortex and arranging equipment inside them according to the optimisation categories allows clinicians to use the equipment itself as a prompt to ensure efficient optimisation of the lifelines. Labels to enable this are available for free download.
gamechangers
Using the structured approach provided by the Vortex, it should be possible to implement all the optimisations required to complete a best effort within three attempts at any lifeline. Despite this, it is recognised that circumstances may occasionally exist where a lack of immediate access to personnel, equipment, or medications might prevent crucial optimisations being implemented within the three attempt limit. In this rare situation, the Vortex Approach provides clinicians with permission to have one additional attempt at a lifeline if an optimisation strategy is considered to be a 'gamechanger'.
To be considered a gamechanger an optimisation strategy must satisfy the following criteria:
It must be reasonably expected to have a profound impact on the probability of entering the Green Zone using the lifeline in question: thus an untried intervention that merely provides another possibility of entering the Green Zone is not considered a gamechanger. The specific interventions likely to have a profound impact
It must not prolong the duration or severity of hypoxia to which the patient is exposed: this will require consideration of the patients oxygen saturations, the immediacy with which the proposed optimisation can be implemented and the likelihood of success of any remaining options to establish alveolar oxygen delivery. Thus in the situation where the patient's oxygen saturations have already fallen, unless the clinician is convinced that the proposed optimisation will provide entry to the Green Zone via the relevant lifeline as fast or faster than the remaining alternatives (residual lifelines or Neck Rescue), it cannot be considered a gamechanger.
“a best effort at any lifeline must include full muscle relaxation”
Examples of interventions that might potentially qualify as 'Gamechangers' in appropriate situations, include the following:
Previously unavailable novel equipment that specifically targets the challenges being faced: this includes devices such as a hyperangulated videolaryngoscope or a straight blade direct laryngoscope (in appropriately skilled hands) but not more subtle variations in the size/type of devices which have already used.
Rectification of equipment failure: where equipment failure (e.g. light failure on laryngoscope, screen/camera failure on videolaryngoscope) has prevented proper execution of a previous attempt and the defect can be corrected by device repair/replacement
Full muscle relaxation: a best effort at any lifeline must include full muscle relaxation (unless this cannot be provided within the necessary timeframe) as this will make FMV, SGA, ETT & Neck Rescue easier.
Another clinician of equivalent or increased experience: in addition to technical prowess, the impact of a 'fresh arm' at direct laryngoscopy should not be underestimated as multiple attempts may have resulted in significant fatigue that has counteracted the impact of other optimisation strategies.
An ENT surgeon proficient in rigid laryngoscopy/bronchoscopy and the necessary equipment to perform this procedure.
None of these interventions should be assumed to automatically qualify as gamechangers. The specific interventions likely to satisfy the above criteria will vary according to the clinical situation and the particular challenges faced. The likely impact of a contemplated optimisation strategy on the factor impeding establishment of alveolar oxygen delivery must be considered in context.
A completed best effort at any lifeline may thus consist of up to three attempts +/- a gamechanger. The use of specific, limited criteria which must be satisfied for the gamechanger to be invoked provides boundaries to ensure accountability for this action and avoid fixation on upper airway lifelines when Neck Rescue is clearly indicated.
Human factors
Most of the major difficult airway algorithms emphasise the need to make declarations of "failure" at each of intubation, supraglottic airway and face mask ventilation in order to facilitate team situational awareness of the need to move on to other techniques. Declaring that alveolar oxygen delivery cannot be achieved by a given technique is a key step in encouraging the team to commit to alternate strategies but linking such a declaration to the notion of "failure", with the implications this may carry for the competence of the airway operator, has the potential to become a barrier to such a declaration being made.
Richard Levitan has spoken about the importance of psychology in approaching transition to Neck Rescue and the concept of the "surgically inevitable airway", stressing the need to move away from the perception that the need to perform this procedure indicates inadequacy on the part of the airway clinician. The challenges presented managing any airway are the culmination of patient anatomy, circumstances and clinician factors. While clinician factors certainly include planning and clinical skills (and where these are inadequate they may certainly contribute to the need for Neck Rescue when it could otherwise have been avoided) focusing on this aspect during the transition process is of no conceivable benefit. Faced with an evolving airway crisis the team must do their best within the context they find themselves in. The psychological burden of declaring "failure" has the potential to become an impediment to effective transition even for clinicians who have performed exceptionally and are simply unlucky enough to find themselves presented with the "surgically inevitable airway".
In keeping with this principle, the endpoint of attempts to establish alveolar oxygen delivery via any lifeline using the Vortex Approach is declared by the team as a "completed best effort". This term serves to convey the futility of further attempts at the relevant lifeline while emphasising that the clinician has maximised the the opportunities available to them according to anatomical, situational and clinician factors at the time. The expectation is that there are less barriers to a clinician to declaring a "completed best effort" at intubation than to declaring "failure". If following a completed best effort at any lifeline alveolar oxygen delivery has not been restored, then alternate strategies must be pursued, including Neck Rescue when best efforts at all upper airway lifelines have been exhausted.